Why Do Some Cultures Withhold Terminal Diagnoses from Patients?
Exploring the cultural reasons behind why some societies choose not to disclose terminal diagnoses directly to patients, and how this impacts patient autonomy and family dynamics.
10/27/20243 min read


Why Do Some Cultures Withhold Terminal Illness Diagnoses from Patients?
In countries like Australia, the UK, and the USA, not informing a patient of a terminal diagnosis is considered unethical. Here, medical ethics emphasize self-determination, ensuring patients can make informed decisions about their care. However, this practice varies globally, especially in collectivist cultures, where not informing the patient is seen as a protective measure. Let’s explore the reasons behind this difference, contrasting individualistic and collectivist approaches to patient care.
Watch Our Full Video Here:
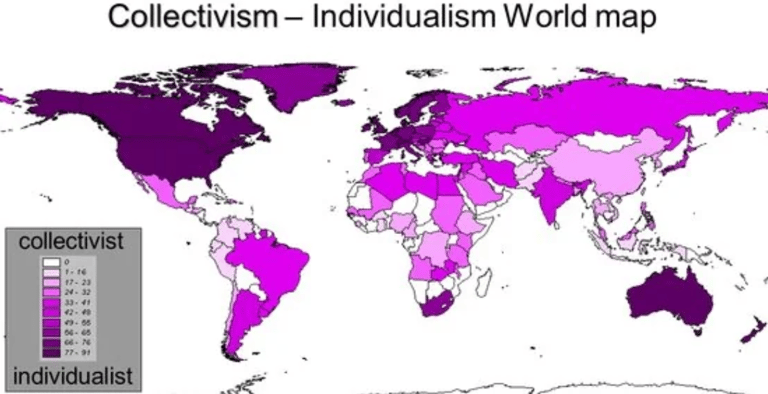
Individualistic vs. Collective Cultures
Individualistic Cultures
In countries like Australia, the USA, Canada, and Germany, individualistic cultures prioritise personal choice and self-expression. People in these cultures, where privacy, independence, and self-dependence are highly valued, often see themselves as loosely connected to others and driven by personal goals. This focus on autonomy extends to healthcare, where patients expect to be informed and actively involved in their medical decisions.
Despite its strengths, individualism can lead to challenges, such as elderly parents and disabled individuals receiving less family support. In medicine, this approach prioritizes personal autonomy and decision-making, valuing each patient’s right to be informed about their own health.
Collectivist Cultures
In contrast, collectivist cultures, like those in China, Japan, India, and Ghana, place a strong emphasis on the group’s needs over individual desires. Here, personal identity is deeply interconnected with family and community. Such cultures emphasize loyalty, indirect communication to avoid conflict, and decision-making that benefits the group rather than just the individual.
In healthcare, this often means that families, rather than the patient alone, handle medical decisions. The goal is to shield the patient from stress, viewing this protective measure as an act of kindness. While this approach has benefits, it can create challenges, especially for those who wish to play an active role in their healthcare.
Real-World Example: Chinese Culture and Patient Care
An example of this cultural difference in practice comes from Chinese healthcare. In China, it is common for doctors to share serious diagnoses with family members rather than the patient. Discussing death is considered unlucky, so families often decide how much information to share with the patient. For instance, Ms. Z, an elderly Chinese woman in a U.S. hospital, had her health information managed by her son. Even when her health outlook was poor, her son preferred that she not be informed, hoping to keep her spirits up while he managed the necessary medical decisions.
What Do Patients Really Want?
Studies in collective societies, including Turkey, Iran, and Greece, have revealed that patients often want more information than families assume. Researchers found that younger patients generally wanted to be involved in their healthcare, and women were more likely to have their diagnoses withheld by relatives. Additionally, many patients expressed a desire to prepare spiritually, a need often unmet due to lack of information about their condition.
While families may believe they are sparing loved ones from stress, some healthcare professionals argue this approach can be more self-serving than protective. A better balance, suggested by many patients, would involve family support for daily decisions, while the patient manages larger, life-altering choices.
Considering Terminal Illness in Children
This topic also applies to terminally ill children, with some parents choosing not to disclose their child’s diagnosis. Although less common in Western countries, this choice is sometimes made with the belief that the child would not understand or that it would be “too much.” However, children, even very young ones, often pick up on cues about their health. Being honest with children, in age-appropriate ways, helps them feel respected and prepared for what lies ahead.
Conclusion: Cultural Perspectives on Patient Autonomy
The ethical approach to delivering a terminal diagnosis varies widely across cultures. While collective cultures prioritise the family’s role in caregiving and decision-making, even patients within these societies increasingly want to know the truth. Balancing respect for cultural norms with individual patient autonomy is essential, and healthcare providers must navigate these nuances with care.
If you’re looking for personal guidance in navigating death and dying related concerns, consider booking a 1-on-1 online consultation with one of our specialists to support your journey.