Ranking U.S. States on End-of-Life Care: The Best & Worst States Revealed
How does your state rank when it comes to end-of-life care? In this blog, we break down the 2024 State-by-State Scorecard on Palliative Care released by the Center to Advance Palliative Care (CAPC) and the National Palliative Care Research Center.
6/30/20254 min read
Which U.S. States Are Best at Dying? A Look at Palliative Care Rankings
A few weeks ago, we explored which countries do death best, based on a global survey from Duke University. That video sparked a wave of interest, with many people asking: “Do they break it down by regions or states?” While Duke’s report didn’t go that far (and even said so), it raised a great question — how do different states within a country rank when it comes to end-of-life care?
So, over the next few weeks, we’ll be diving into the internal data of several countries — beginning with the United States, which, if you recall, came in 43rd globally in that original report.
Today’s post looks at how U.S. states compare when it comes to palliative care access and infrastructure. Spoiler: it's a mixed bag.
What Is Palliative Care and Who Tracks It?
Every few years, the Center to Advance Palliative Care (CAPC) — based at the Icahn School of Medicine at Mount Sinai in New York — collaborates with the National Palliative Care Research Center (NPCRC) to produce a comprehensive report titled:
“America’s Readiness to Meet the Needs of People with Serious Illness: A State-by-State Look at Palliative Care Capacity”
We’re using their 2024 Scorecard for this analysis. You can view the full report here.
Palliative care is not just for the dying — it’s also for those living with serious illness. But most frequently, it’s used by people with terminal diagnoses or those in advanced age. The scorecard evaluates each state on a 5-point scale based on:
Availability of specialty-trained palliative care professionals
Payment structures for services
Public awareness and access mechanisms
Basic education in palliative care for clinicians
Support for caregivers and functional needs
These are basic standards for any modern healthcare system. Not asking for miracles here.
Important Note: Voluntary Assisted Dying (VAD) laws are not included in the rankings. CAPC intentionally left this out to avoid politicizing the scorecard or conflating different end-of-life options. VAD is a separate issue. High-quality palliative care should always be available — regardless of your stance on VAD.
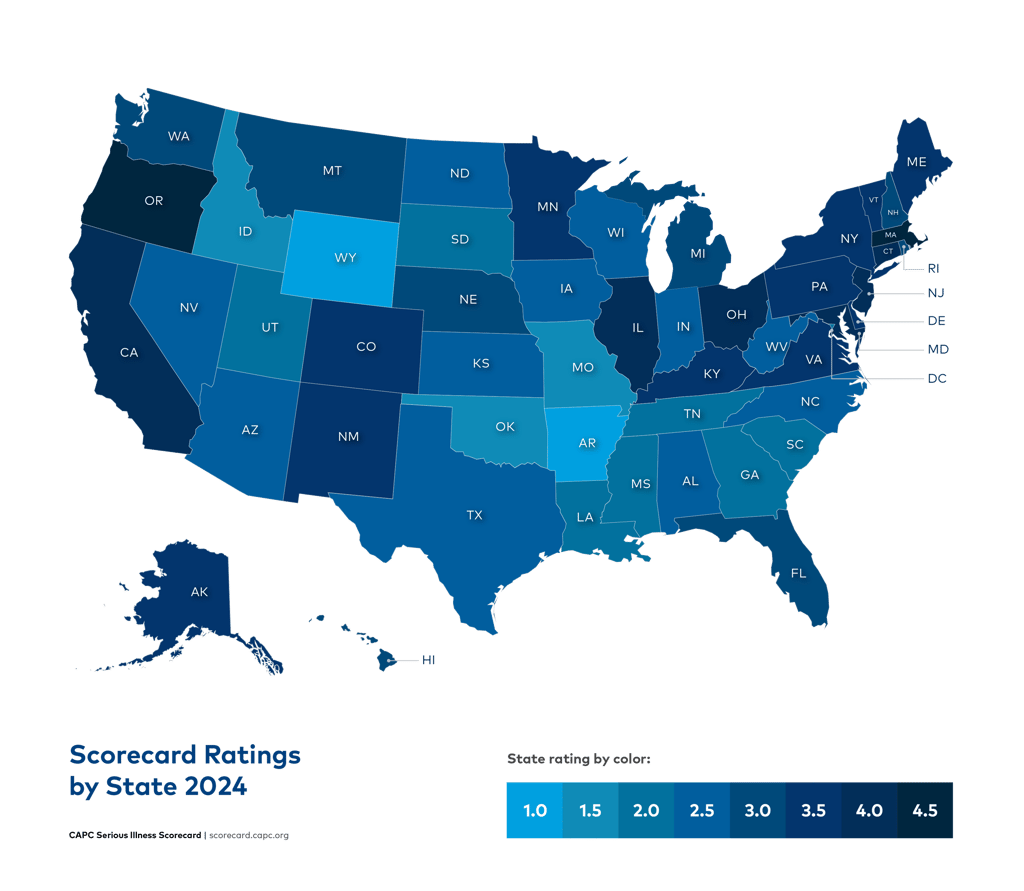
How Did the States Rank?
Before you scroll — take a moment to guess: How do you think your state scored out of 5? Done? Great. Here’s what the report found:
🌟 4.5 Stars (Top Ranking):
Massachusetts
Oregon
🌟 4 Stars:
California
Connecticut
Illinois
Maryland
New Jersey
Ohio
🌟 3.5 Stars:
Alaska
Colorado
Delaware
Kentucky
Maine
Minnesota
New Mexico
New York
Pennsylvania
Vermont
Virginia
🌟 3 Stars:
Florida
Hawaii
Michigan
Montana
Nebraska
New Hampshire
Rhode Island
Washington
⚠️ 2.5 Stars:
Alabama
Arizona
Indiana
Iowa
Kansas
Nevada
North Carolina
North Dakota
Texas
West Virginia
Wisconsin
⚠️ 2 Stars:
District of Columbia
Georgia
Louisiana
Mississippi
South Carolina
South Dakota
Tennessee
Utah
⚠️ 1.5 Stars:
Idaho
Missouri
Oklahoma
🚨 1 Star (Lowest Ranking):
Arkansas
Wyoming
If your jaw dropped, you’re not alone. We were surprised by New York’s middle-of-the-pack placement and Alabama not coming in last — shocking, right? You can view the full score breakdown here.
What’s Happening With U.S. Hospitals?
One part of the report that stood out: the U.S. is rapidly losing hospitals. In fact, nearly every state has fewer hospitals in 2024 than it did in 2019. For example:
Alabama: 56 → 28 hospitals
Illinois: 103 → 79
North Carolina: 74 → 52
This decline is mostly due to rural hospital closures, largely because insurance companies pay them far less than urban hospitals for the same services. That’s a big problem — especially since rural hospitals are already less likely to offer palliative care.
On the flip side, the number of hospitals with palliative care teams has improved overall, which is good news. In some states, 100% of hospitals now have palliative care programs, including:
Alaska
Delaware
Maryland
New Hampshire
North Dakota
Rhode Island
Utah
Vermont
Other states like Ohio and New Jersey are close behind.
Full data on hospital coverage is here.
Who’s Doing the Heavy Lifting? Hospital Types Matter
Let’s break it down by hospital type:
🏥 For-Profit Hospitals
Goal: Generate profit for investors
Funding: Primarily through insurance/patient payments
Palliative Care Access: 49%
🏥 Nonprofit Hospitals
Goal: Reinvest profits into services
Funding: Insurance + major donations/philanthropy
Palliative Care Access: Highest among all types
🏥 Public Hospitals
Goal: Serve vulnerable populations
Funding: Mix of insurance, government subsidies, and grants
Access: Variable, but often a safety net
The report confirms: for-profit and rural hospitals are least likely to offer palliative care. That’s a major equity issue.
The Workforce Problem
According to the scorecard, the U.S. has only 19,920 certified hospice/palliative care clinicians, with just 2.86 prescribers per 100,000 people. That’s alarmingly low.
Why? Palliative care isn’t a highly paid or “glamorous” specialty. But there is a positive trend: the CAPC is pushing for basic palliative care training for all healthcare professionals — not just specialists.
22 states now require continuing education in end-of-life care for medical licensure.
136,000+ professionals have completed CAPC’s online training in communication, pain management, dementia care, and more.
This wider education approach is working — and it’s key to reducing the over-medicalization of dying and helping healthcare workers handle death better.
Final Thoughts
America’s end-of-life care picture is complicated. Some states are doing well, others are drastically underperforming. But the direction is hopeful, thanks to organizations like CAPC pushing for progress.
What should you do?
Don’t wait until you're dying to make plans.
Learn what’s available in your state.
Have conversations with your loved ones.
Make your wishes known in advance.
We’ll be covering Australia’s state-by-state rankings next, so be sure to check back or subscribe on YouTube for updates.
Until then — go talk death.
Resources:
Want to go deeper?
We offer consultations and tailored education sessions exploring death, trauma, cultural narratives, and how to talk about difficult topics. Whether you’re an educator, student, or simply curious — we’re here to help you navigate these conversations with care and depth.
🎁 Download our digital resources – a mix of practical tools and in-depth guides on grief, mental health, and supporting others through difficult times.
🧠 Book a one-on-one session – talk with a professional in a safe, compassionate space